Noble beginnings
Many consider Johns Hopkins Hospital to be a world-class institution.
It certainly aims to be with an institutionally declared mission
statement “to improve the health of our community and the world by
setting the standard of excellence in patient care.”
The hospital’s beginning hails back to 1889, along with a medical
school and nursing school, commissioned by its benefactor, Johns
Hopkins. Hopkins set forth this mission on his deathbed with
instructions and funds to create a hospital to “treat the poor without
charge,” no matter the patient’s “age, sex, or color.” He embraced this
edict as both obligation and opportunity to provide aid to the poor
and improve the social standards of his community in keeping with
his family’s Quaker beliefs.
At the time, the institution was groundbreaking in providing care to
the poor and, in particular, poor children of color. Combining patient
care and research alongside formal nursing and medical education
led to many benets for the people of Baltimore as well as to the
development of both the nursing and medical professions. These early
beginnings, and adherence to the ideals underlying the vision of Johns
Hopkins, are the basis upon which Johns Hopkins Hospital obtained
its stellar reputation.
Johns Hopkins Hospital:
REALITY vs.
REPUTATION
www.NationalNursesUnited.org
On his deathbed, Johns Hopkins set forth
instructions and funds for the creation of a
hospital that would serve this purpose:
“to treat the poor without charge”
no matter the patient’s “age, sex, or color.”

Reality falls short of reputation
Nurses are drawn to employment at Johns Hopkins
Hospital for the prestige and opportunity to practice
nursing at one of the largest academic hospitals on
the East Coast. JHH provides nurses with the ability
to practice in a high-skilled setting providing care to
patients with a variety of complex and uncommon
conditions. Despite this, the reality of working at Johns
Hopkins Hospital is far removed from the picture
described in marketing and recruitment materials.
It is clear to nurses that the current executive leaders
of Johns Hopkins Hospital have lost sight of the early
vision of its founder. Nurses consistently experience
barriers to providing the type of highly skilled and
technical nursing care that all patients deserve —
the kind of care that attracts patients to choose
Johns Hopkins.
The challenges that nurses face in advocating for their
patients and providing safe care are a result of the
administration’s conicting values when prioritizing
and allocating resources. These compromises made at
the expense of patients and care providers are dictated
by executives, far removed from the realities of patient
care, to save money and increase revenues.
Nurses document patient care
concerns in new report
Direct-care RNs who practice at Johns Hopkins
Hospital have written a report to bring attention to
patient safety concerns that they and their patients
face every day. The report, “Foundations of Care:
Upholding the Legacy of Hopkins’ Nurse Pioneers–
Johns Hopkins Hospital Patient Care Report,”
contains a unit-by-unit survey of hospital conditions
and is based entirely on the nurses’ rst-hand
experiences and observations.
KEY FINDINGS
» Patient safety is compromised by high turnover
among registered nurses and lack of experienced
nurses. RN turnover is creating a patient care crisis.
» On many units, there are not enough RNs and
support staff to meet individual patient care needs.
» Necessary supplies, equipment, and protective
gear are often not available, creating delays in care
that pose a risk to the safety of patients and nurses.
Supply shortages are widespread throughout
the hospital and vary from specialty unit to
specialty unit.
» Systemic failure to plan for increases in patient
population, acuity, and intensity creates conditions
that leave patients vulnerable for missed care and
care left undone.
» Poor working conditions: There is no system in
place for break relief, creating conditions that cause
fatigue, stress, and burnout.
» Dysfunctional organizational culture that has
created an atmosphere of fear, frustration,
and futility.
ARE NURSES SAFE AT
JOHNS HOPKINS HOSPITAL?
A survey conducted earlier this year
by Johns Hopkins nurses found:
37% of Hopkins nurses report
that they have experienced
workplace violence in the past year.
50.1% of nurses report that
their concern was ignored or
nothing happened after reporting.
95% of Hopkins nurses replied
that they feel at risk for injury at
work at least sometimes.
» SHORT STAFFING/FAILURE TO PLAN
Adult Emergency Department Wait times (to receive care)
are unsafe on most days, sometimes reaching up to 18 hours in
the waiting room…Oncology patients, patients with chest pain,
patients actively vomiting are just some of the patients left for
many hours to wait. Nurses report that patients have had seizures
in the waiting room, loss of consciousness from bleeding, and
cardiac arrests while waiting for a treatment bed in the main area
of the department.
» TURNOVER
The Surgical Oncology Unit (Weinberg 4CD)
is at a crisis point. Over the last year, almost
50% of the nursing sta has left the floor
with most nurses leaving the hospital entirely.
It is very dicult to retain nurses on the
Pediatric Intensive Care Unit (PICU). It
is common for an RN with one and a
half years of experience to be the most
experienced nurse on a shift. This collective
lack of experience is dangerous for patients
and places nurses in dicult situations in
which they have to take assignments they
are not confident in performing.
» SHODDY EQUIPMENT/
INADEQUATE SUPPLIES
The gloves in the Comprehensive
Transplant Unit (Zayed 9W) are known to
rip. Gloves that are sturdy are especially
important on the CTU because they care
for patients with dierent communicable
diseases (e.g., HIV, hepatitis B and C) and
patients who receive medications with
hazardous handling precautions (e.g. anti-
rejection medicines), and it is unsafe for
nurses to be exposed to the blood and
other bodily fluids of these patients.
The Surgical Intensive Care Unit
(Weinberg 3A) reports that infusion
pumps that are used to administer pain
medication via the Patient Controlled
Analgesia (PCA) protocols are also in
short supply. These PCA pumps oer
a timely and safe delivery method
that avoids overdose for administering
potentially dangerous pain medications
to patients needing frequent relief from
extreme pain, such as that caused by
sickle-cell crisis.
Excerpts from the Johns Hopkins nurses’
patient care report »»»
For more details consult the full report, “Foundations
of Care: Upholding the Legacy of Hopkins’ Nurse
Pioneers– Johns Hopkins Hospital Patient Care
Report,” National Nurses Organizing Committee/Johns
Hopkins RNs.

—Mary Adelaide Nutting,
Johns Hopkins
Superintendent of Nursing
1894-1907
It is a bad day for our schools, for our
nurses, for physicians, and for sick
people everywhere, when the first
question is always, “How little can we
do it for?” rather than “how well can
we do it?”
Johns Hopkins reaps more than it sows from huge tax exemptions
Johns Hopkins Hospital is a not-for-prot hospital, a designation that provides them with exemptions from a large
number of federal, state, and local taxes. In exchange for these tax exemptions, surplus revenues from the not-for-
prot hospital are supposed to benet the community in which it is located.
In a recent report, “Breaking the Promise of Patient Care: How Hopkins Hospital Management Shortchanges
Baltimore and Puts Patients and the Community at Risk,” researchers found that the hospital receives far more in
annual tax exemptions and public funding than they pay out in charity care and community benets.
KEY FINDINGS
» Thanks to the state of Maryland’s unique rate support system that provides Johns Hopkins and other hospitals
public funding, in scal year 2017 Johns Hopkins Hospital paid nothing in charity care from its own resources, and
far less from its own resources in community benets than is commonly believed.
» In scal year 2017 Johns Hopkins Hospital received $24,954,381 in charity care rate support (i.e. public funding)
from the state of Maryland, and spent just $21,697,000 on charity care, leaving it with a surplus of $3,257,381.
» Johns Hopkins Hospital also did not pay more for charity care than it received in rate support in three prior scal
years. When combined for the scal years 2013 through 2017, Johns Hopkins Hospital received $33,091,494 more
in rate support than it paid for the charity care it reported.
» The total loss to the public for scal year 2017 with respect to charity care, or the charity care provided from Johns
Hopkins Hospital’s own resources minus the total value of the tax exemptions, is estimated to be $167,662,220.
» Johns Hopkins track record in providing charity care when compared to other Maryland hospitals is abysmal.
Between 2014 and 2017, Johns Hopkins Hospital was one of the lowest ranked hospitals, providing the least charity
care relative to rate support received. It ranked 49 out of 52 in 2017, 51 out of 52 in 2016, 53 out of 53 in 2015, and
49 out of 52 in 2014.
RNs organize to uphold legacy of
Hopkins’ nurse pioneers
Johns Hopkins nurses organizing today, to improve
patient care and hold the institution accountable
to its mission, are inspired by Hopkins’ nurse
pioneers, Isabel Hampton Robb, Mary Adelaide
Nutting, and Lavinia Dock. These early founders
of nursing education and nursing practice at Johns
Hopkins Hospital are recognized not only for their
academic prowess and clinical skills, but also for their
commitment to social justice advocacy, which could be
viewed as an extension of the profession’s core values.
Together, this “extraordinary triumvirate of women”
shared a commitment to the most challenging social
issues of their time, such as women’s suffrage, the
abolition of slavery, and improving living conditions
for the poor. A deep understanding of the social
determinants of health led them to be advocates far
beyond the walls of the nursing school and the hospital.
Baltimore remains one of the poorest, large cities in the
United States with an estimated poverty rate of 23.1
percent for 2017. In scal year 2017, only 0.6 percent of
Johns Hopkins’ patients were uninsured despite the fact
that Baltimore’s uninsured rate is 9 percent. Of 47,703
inpatient admissions, just 284 patients were uninsured.
1
Johns Hopkins Hospital would have needed to see
4,266 uninsured patients in FY 2017 for its uninsured
admissions to match the current uninsured rate of the
city of Baltimore, something it fell far short of despite its
location in East Baltimore.
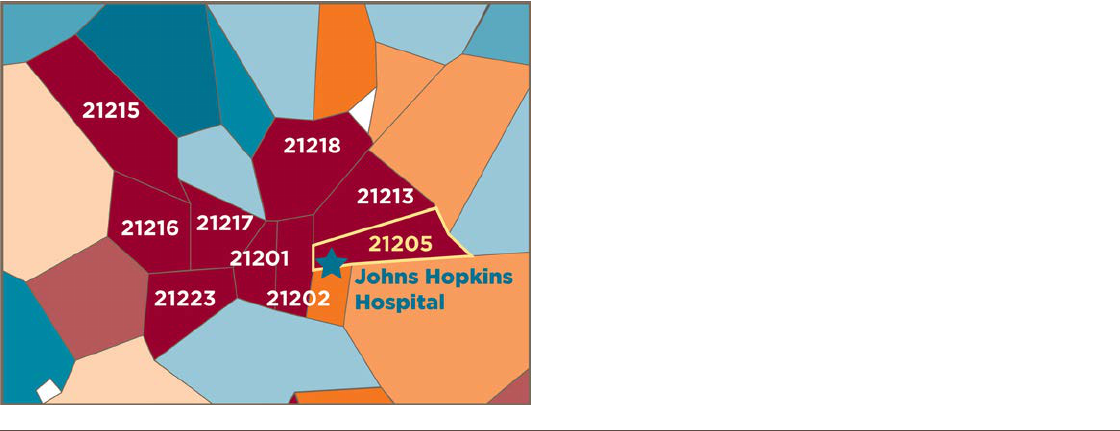
The zip code that surrounds Johns Hopkins Hospital
on three sides is 21205, a zip code with an estimated
poverty rate of 38.6 percent, and one of the most
distressed zip codes in America, ranked in the 93rd
percentile, with 100 percent being the most distressed
(see gure 1).
2
The Old Town/Middle East neighborhood where Johns
Hopkins Hospital is located has an infant mortality rate
of 12.6 per 1,000 live births, 217 percent higher than the
infant mortality rate for the United States as a whole
(5.8 per 1,000 live births).
3
The neighborhood’s infant
mortality rate is roughly equal to the rate for Malaysia,
which is ranked 115 of 225 countries.
4
Both China and
Mexico have lower infant mortality rates than the Old
Town/Middle East neighborhood.
5
Life expectancy in
the Old Town/ Middle East neighborhood is just 70.4
years, 9.6 years lower than the 80 years of the United
States as a whole, and equal to the life expectancy in
Turkmenistan, ranked 159 out of 224 countries.
6
This brochure contains information drawn from:
“Breaking the Promise of Patient Care: How Hopkins Hospital Management Shortchanges Baltimore and Puts
Patients and the Community at Risk.” Produced by National Nurses United and AFL-CIO. December 2018.
Available at www.nationalnursesunited.org/nnocnnu-campaign-literature
“Foundations of Care: Upholding the Legacy of Hopkins’ Nurse Pioneers – Johns Hopkins Hospital Patient Care
Report.” Based entirely on rst-hand experience and observations of direct-care RNs employed by Johns Hopkins
Hospital in Baltimore. National Nurses Organizing Committee/Johns Hopkins RNs. December 2018.
Available at www.nationalnursesunited.org/nnocnnu-campaign-literature
End Notes
1. Maryland Health Services Cost Review Commission, Community Benets Program, Maryland Hospital Community Benet Report: FY 2017 https://hscrc.maryland.gov/Pages/
init_cb.aspx, accessed 8/09/17.
2. Economic Innovation Group, Distressed Communities Index (DCI), 2017, DCI Data for U.S. Zip Codes.
3. Baltimore City Health Department, Baltimore City 2017 Neighborhood Health Prole, Old Town/Middle East, https://health.baltimorecity.gov/sites/default/les/NHP%20
2017%20-%2041%20Oldtown-Middle%20East%20 (rev%206-9-17).pdf
4. CIA, The World Factbook Country Comparison: Infant Mortality Rate, https://www.cia.gov/library/publications/the-world-factbook/rankorder/2091rank.html, accessed 8/21/18.
5. Ibid.
6. Baltimore City Health Department, Baltimore City 2017 Neighborhood Health Prole Old Town/Middle East, https://health.baltimorecity.gov/sites/default/les/NHP%20
2017%20-%2041%20Oldtown-Middle%20East%20 (rev%206-9-17).pdf
CIA, The World Factbook Country Comparison: Life Expectancy at Birth, https://www.cia.gov/library/publications/the-world-factbook/rankorder/2102rank.html accessed
8/21/18.
There is a tremendous need for charity care in Baltimore, especially in
Johns Hopkins’ own neighborhood!
FIGURE 1. Zip codes in red are zip codes that are judged to be in
the 90th percentile for distress, or more distressed than 90 percent
of other U.S. zip codes.

Sign the Petition
Join the Johns Hopkins Nurses’ Call for Change!
www.NationalNursesUnited.org
We, the undersigned nurses,
patients, and community members
call on Johns Hopkins Hospital’s management to live
up to the institution’s world-renowned reputation of
excellence. We recognize that, historically and to this
day, JHH management has fallen short of this reputation.
To begin to repair this harm, we call on JHH
management to:
1. Declare and return the millions of unused and/or
misused dollars in rate support they receive under
the auspices of charity care to their patients and to
the East Baltimore community they have promised
to serve.
2. Listen to and implement all of the patient care
recommendations put forth by nurses organizing to
improve care for JHH’s patients.
3. Terminate their anti-union consultants and allow nurses
to freely organize a union that can advocate on behalf
of themselves, their patients, and our community.
Learn more about Johns Hopkins nurses’ union organizing campaign by visiting:
www.nationalnursesunited.org/johns-hopkins-rns-speak-out
Find us on Facebook at Hopkins Nurses United to learn of upcoming events!
To read and sign the full petition visit:
www.nationalnursesunited.org/johns-hopkins-hospital-petition
