Emergency Care
CHAPTER
Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
THIRTEENTH EDITION
Musculoskeletal Trauma
28

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
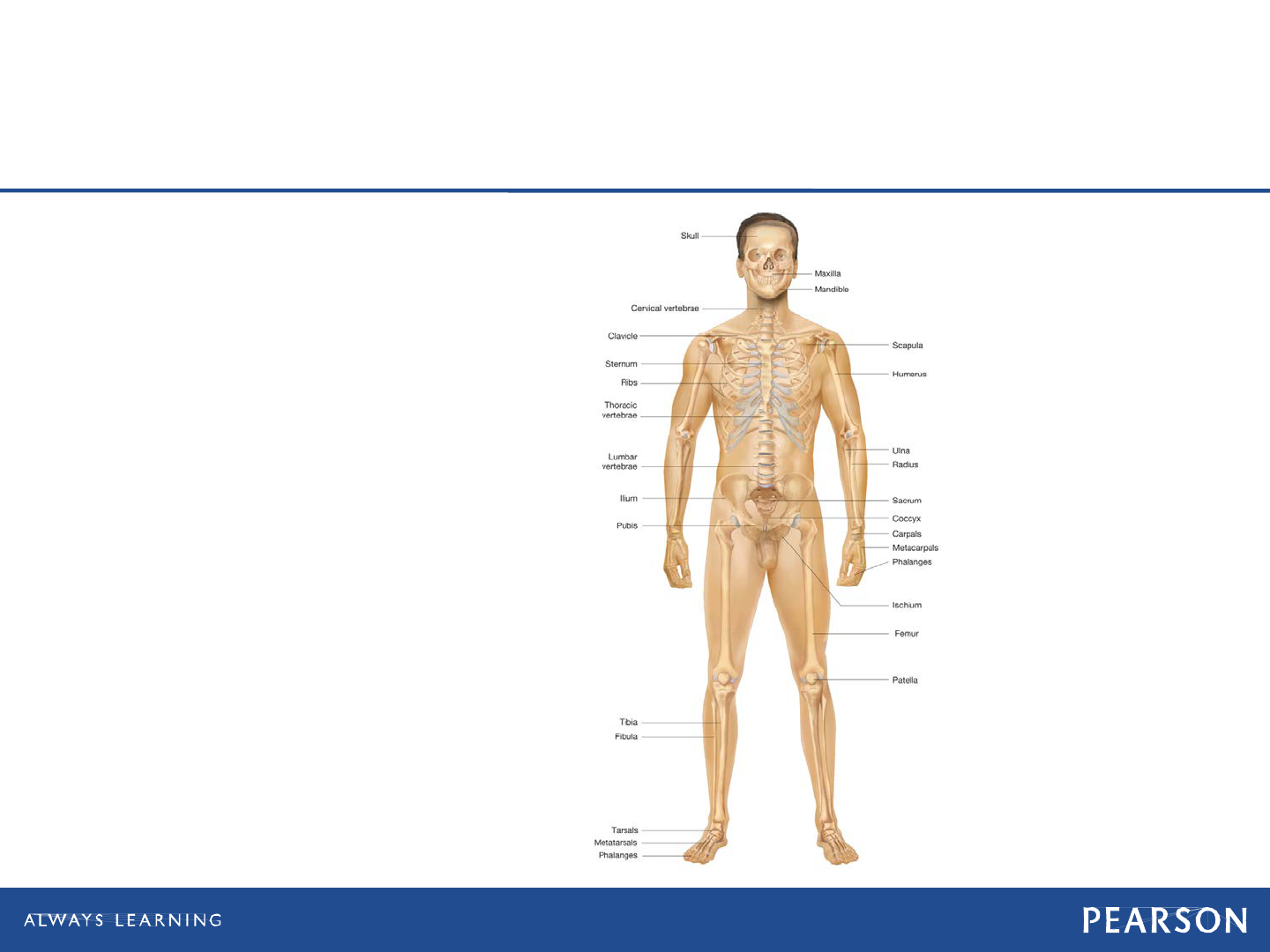
Musculoskeletal System
Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Musculoskeletal System
• Bones
Framework
• Joints
Bending
• Muscles
Movement
continued on next slide

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
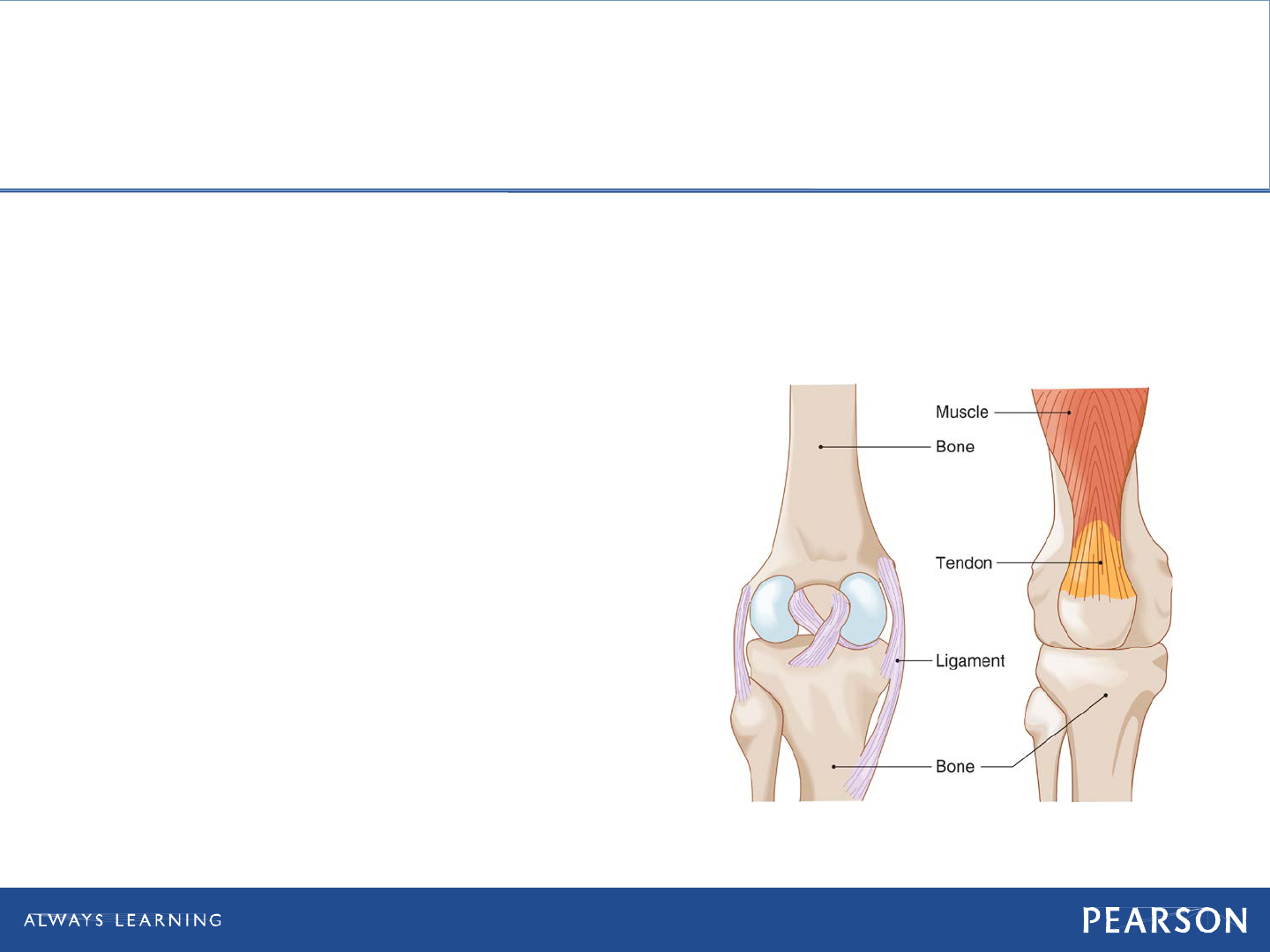
Musculoskeletal System
• Cartilage
Flexibility
• Ligaments
Connect bone to bone
• Tendons
Connect muscle to bone

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Anatomy of Bone
• Bones
Formed of dense connective tissues
Vascular and susceptible to bleeding on
injury
Covered by periosteum
Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
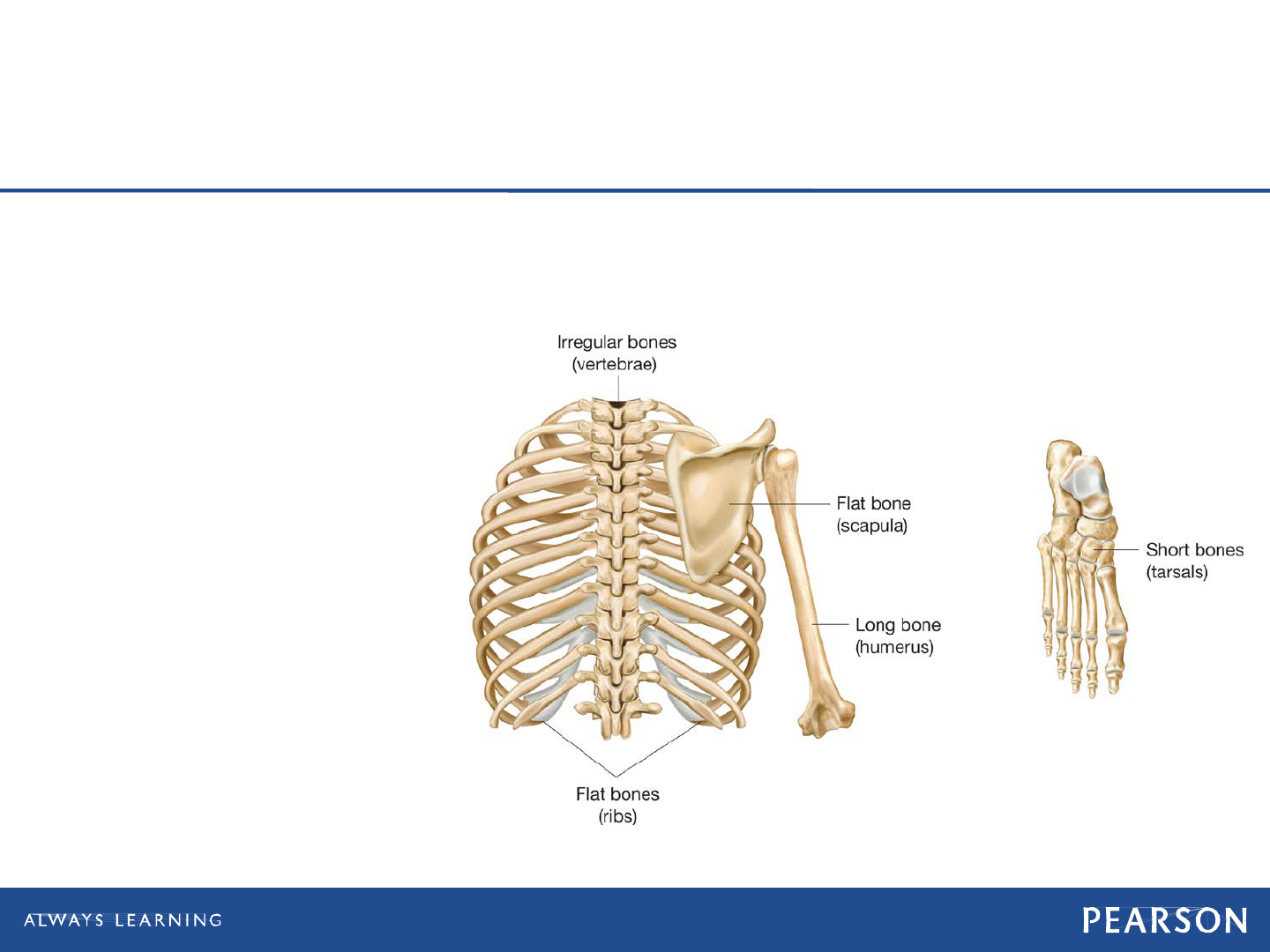
Anatomy of Bone
• Classification of shape
Irregular
Long
Short
Flat
Bones are classified by shape.

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Self-Healing Nature of Bone
• Break causes soft tissue swelling and a
blood clot in the fracture area.
• Interruption of blood supply causes
cells to die at injury site.
• Cells further from fracture rapidly
divide forming tissue that heals the
fracture and develops into new bone.
Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
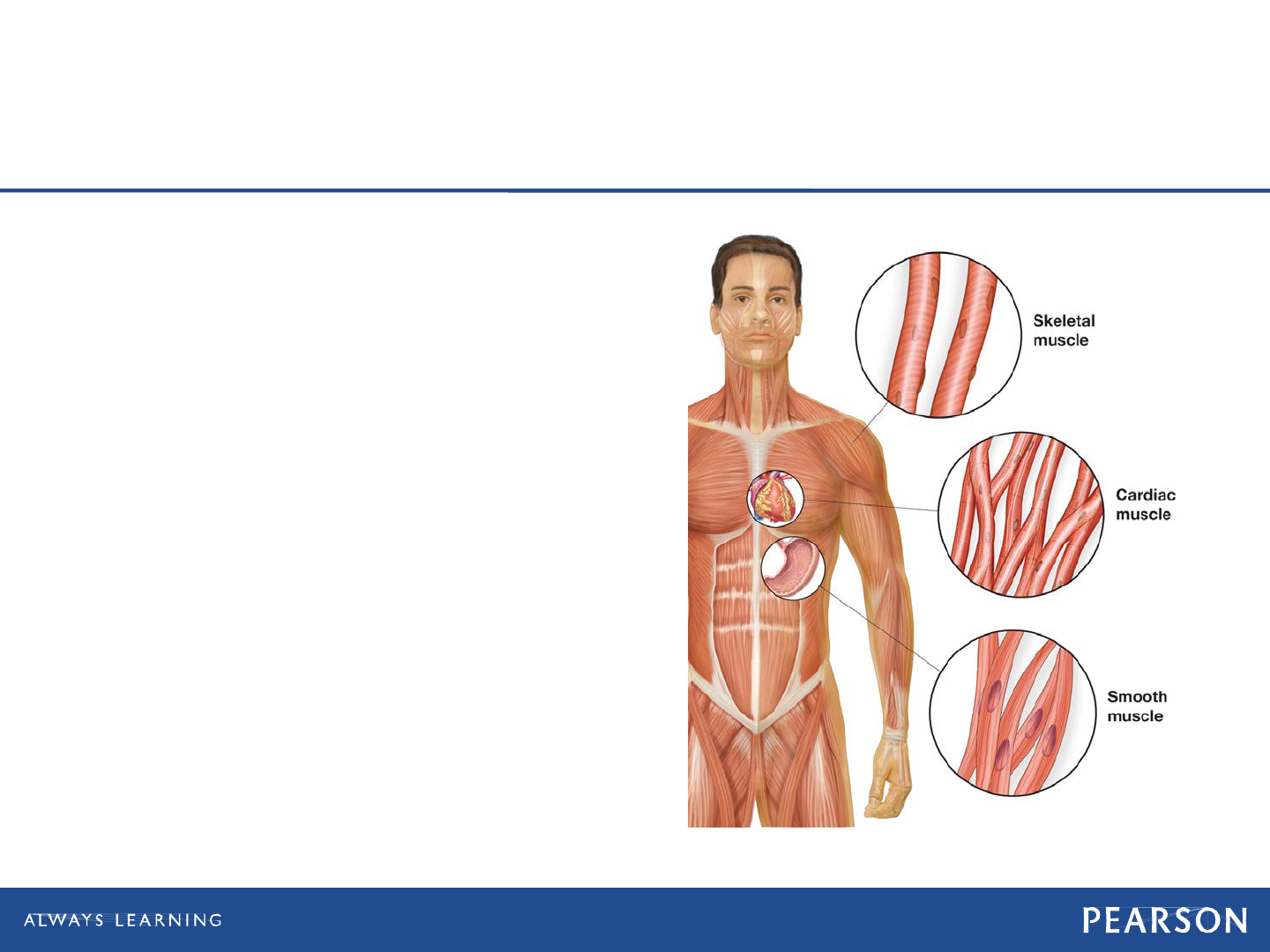
Muscles
• Kinds of muscles
Skeletal (voluntary)
Smooth (involuntary)
Cardiac (myocardial)

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Cartilage
Cartilage helps form flexible structures of
the body.
Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
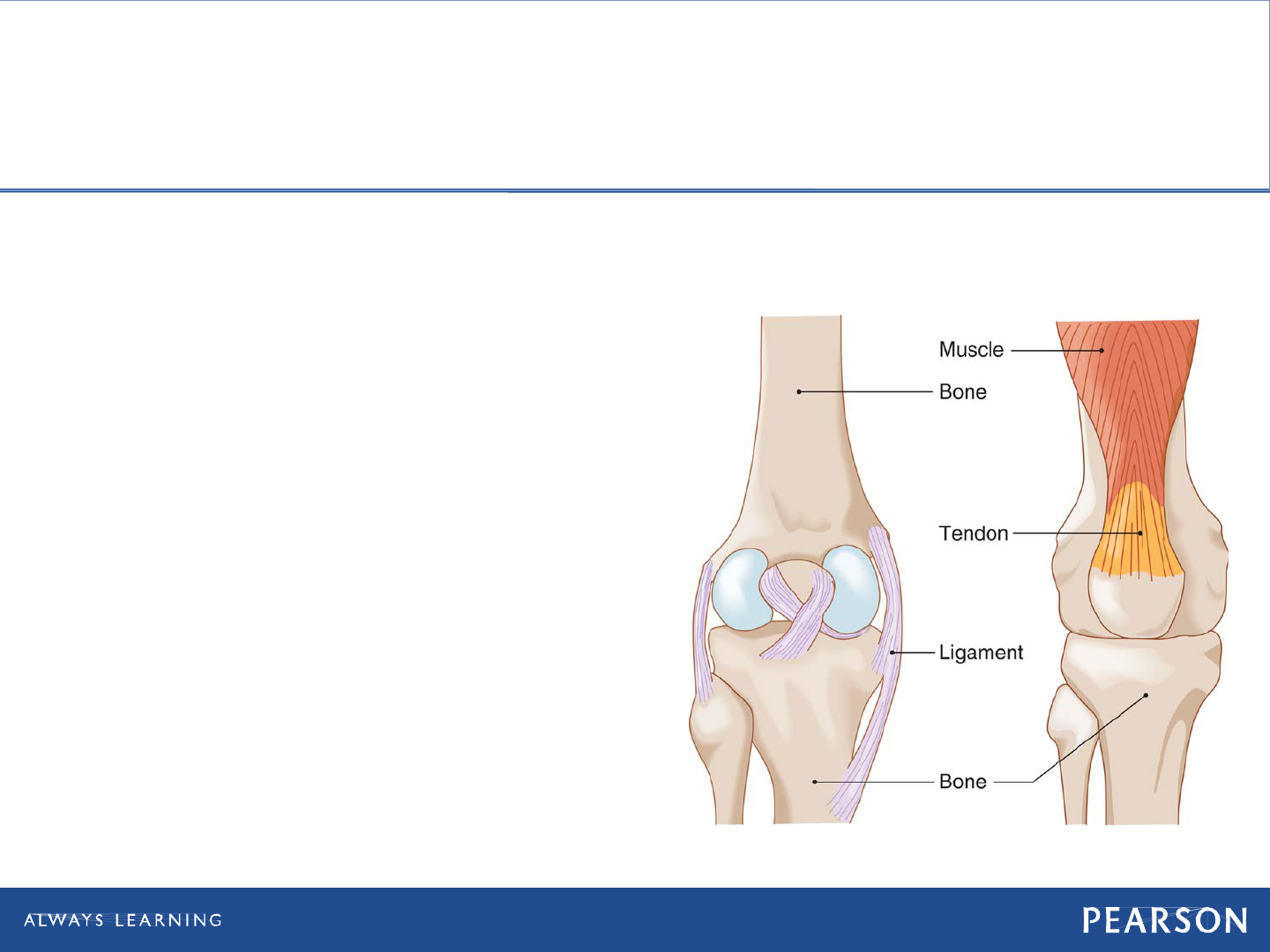
Ligaments
Tendons tie muscle to bone. Ligaments tie bone to bone.
Ligaments support joints by attaching bone
ends to allow for stable range of motion
BLB = bone-ligament-bone
Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Tendons
Tendons tie muscle to bone. Ligaments tie bone to bone.
Tendons allow for the power of movement
across joints.
MTB = muscle-tendon-bone

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
General Guidelines for
Emergency Care

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Mechanisms of
Musculoskeletal Injury
• Direct force
• Indirect force
• Twisting (rotational) force

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Injury to Bones and
Connective Tissue
• Fracture
Any break in a bone, open or closed
Comminuted
• Broken in several places
Greenstick
• Incomplete break
Angulated
• Bent at angle

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Injury to Bones and
Connective Tissue
Closed fracture. © Edward T. Dickinson, MD

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Injury to Bones and
Connective Tissue
• Dislocation
"Coming apart" of a joint
• Sprain
Stretching and tearing of ligaments
• Strain
Overstretching or overexertion of
muscle
continued on next slide

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Injury to Bones and
Connective Tissue
• Not all injuries can be confirmed as a
fracture in the field.
• Splinting an extremity with a suspected
fracture helps prevent blood loss from
bone tissues.

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Assessment of
Musculoskeletal Injuries
• Rapidly identify and treat life-
threatening conditions.
• Be alert for injuries besides grotesque
wound.
• Cut or remove patient's clothing to
complete examination according to the
environment and severity of situation.

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Compartment Syndrome
• Severe swelling in the extremity as a
result of fracture
• Progression
Fracture or crush injury causes bleeding
and swelling in extremity.
Pressure and swelling become so great
the body can no longer perfuse the
tissues against pressure.
continued on next slide

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Compartment Syndrome
• Progression
Cellular damage occurs, causing
additional swelling.
Blood flow to the area is lost.
• Limb may also be lost if the pressure is
not relieved.

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Patient Assessment
• Pain and tenderness
• Deformity and angulation
• Grating (crepitus)
• Swelling and bruising
• Exposed bone ends
• Joints locked into position
• Nerve/blood vessel compromise
• Compartment syndrome
continued on next slide

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Patient Assessment
• Six P's of assessment
Pain or tenderness
Pallor (pale skin)
Parasthesia (pins and needles)
Pulses diminished or absent
Paralysis
Pressure

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Think About It
• Do my patient's musculoskeletal
injuries add up to serious multiple
trauma?
• Does my patient have circulation,
sensation, and motor function distal to
the suspected fracture or dislocation?

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Patient Care
• Take Standard Precautions.
• Perform primary assessment.
• During secondary assessment, apply
cervical collar if you suspect spine
injury.

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Patient Care
• Splint any suspected extremity
fractures after treating life-threatening
conditions.
• Cover open wounds with sterile
dressings.

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Splinting
• Advantages
Minimizes movement of disrupted joints
and broken bone ends
Prevents additional injury to soft tissues
• Nerves, arteries, veins, muscles
Decreases pain
Minimizes blood loss
Can prevent a closed fracture from
becoming an open fracture
Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Realignment of the
Deformed Extremity
• Assists in restoring effective circulation to
extremity and to fit it to splint
• If not realigned, splint may
be ineffective, causing
increased pain and possible
further injury.

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Realignment of the
Deformed Extremity
• If not realigned, increased chance of
nerves, arteries, and veins being
compromised
• Increased pain is only momentary.
continued on next slide

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Realignment of the
Deformed Extremity
• Guidelines
One EMT grasps distal extremity while
partner place one hand above and
below injury site.
Partner supports first EMT who creates
gentle manual traction in direction of
long axis of extremity.
If no resistance is felt, maintain gentle
traction until extremity is properly
aligned and splinted.

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Strategies for Splinting
Splints and accessories for musculoskeletal injuries.

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Strategies for Splinting
• Effective splinting may require some
ingenuity.
• Three types available on EMS units
Rigid splints
Formable splints
Traction splints

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Strategies for Splinting
• Care for life-threatening problems first.
• Expose injury site.
• Assess distal CSM.
• Align long-bone injuries to anatomical
position.
• Do not push protruding bones back into
place.
continued on next slide

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Strategies for Splinting
• Immobilize both injury site and
adjacent joints.
• Choose splinting method based on
severity of condition and priority
decision.
• Apply splint before moving patient to
stretcher or other location if possible.
• Pad voids.

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Hazards of Splinting
• "Splinting patient to death"
Splinting before life-threatening
conditions addressed
• Not ensuring ABC's
• Too tight
Compresses soft tissues
• Too loose
Allows too much movement
• Splinting in deformed position

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Treatment: Splinting Long-Bone
and Joints
First Take Standard Precautions.
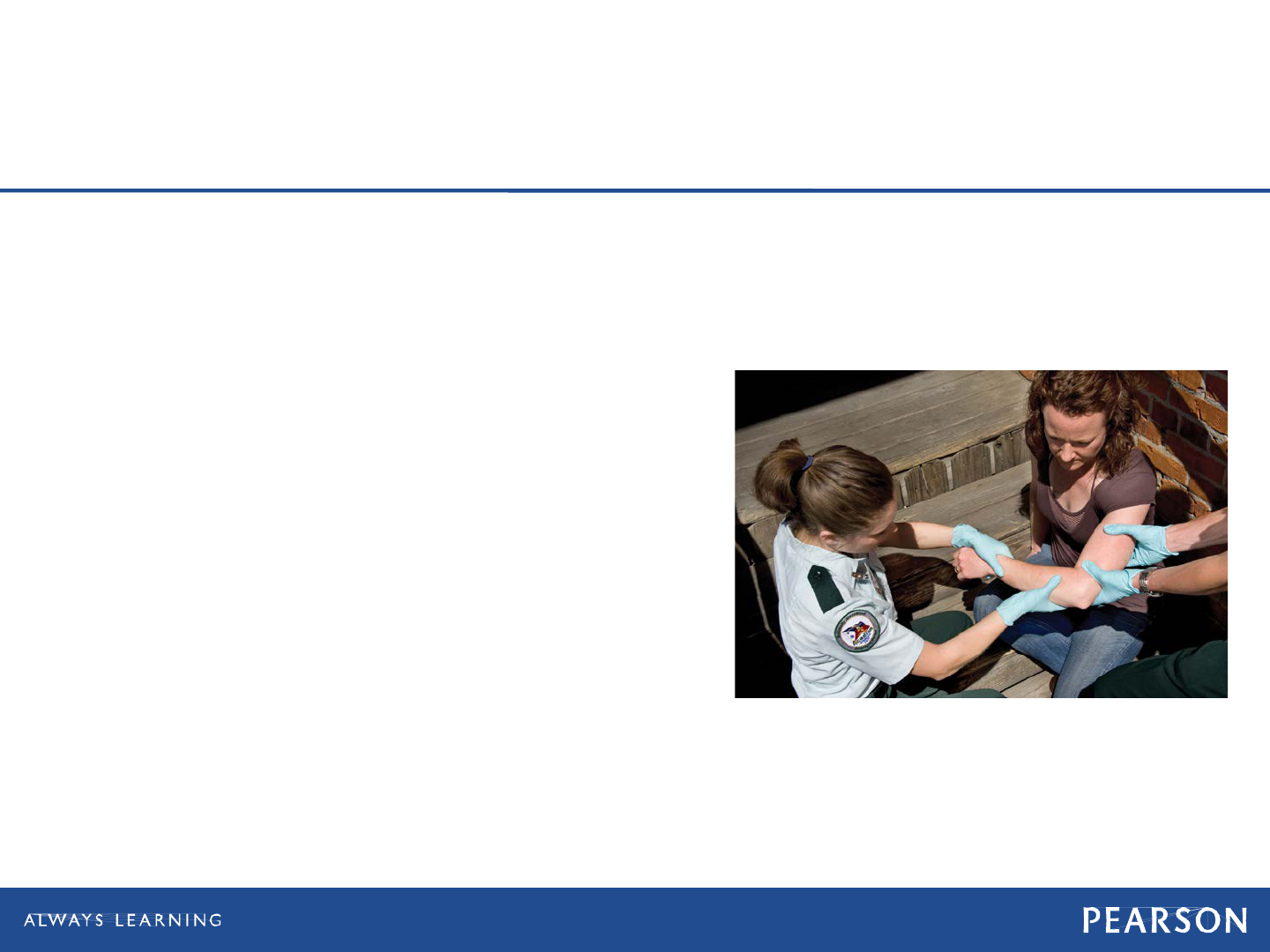
1. Manually stabilize the injured limb, in this case an injured elbow.

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Splinting Long-Bone
and Joint Injuries
• Take appropriate Standard precautions.
• If possible, expose area to be splinted.
• Manually stabilize injury site.

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
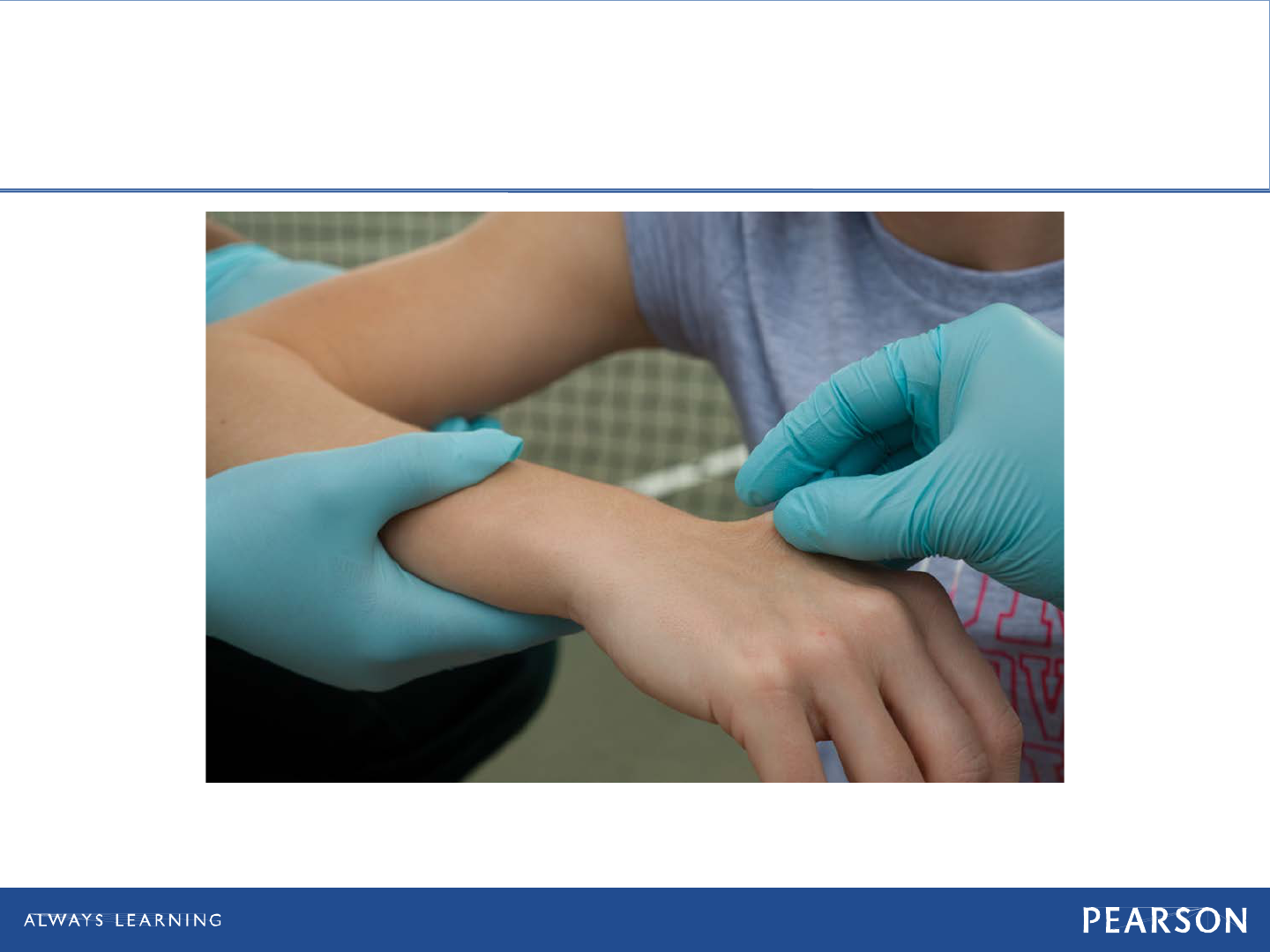
Splinting Long-Bone
and Joint Injuries
• Assess circulation, sensation, and
motor function.
• Realign injury if deformed or if distal
extremity is cyanotic or pulseless.
Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Treatment: Splinting Long-Bone
and Joints
2. Assess distal pulse, motor function, and sensation (CSM).

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Splinting Long-Bone
and Joint Injuries
• Measure or adjust splint.
Move it into position.
• Apply and secure splint to immobilize
injury site, adjacent joints.
• Reassess CSM distal to injury.

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Treatment: Splinting Long-Bone
and Joints
4. Secure the splint.

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Treatment: Splinting Long-Bone
and Joints
5. Reassess distal CSM.

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Traction Splint
• Counteracts muscle spasms and greatly
reduces pain
• Types
Bipolar
Unipolar
• Amount of traction applied should be
roughly 10 percent of patient's body
weight
Not exceeding 15 pounds
continued on next slide

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
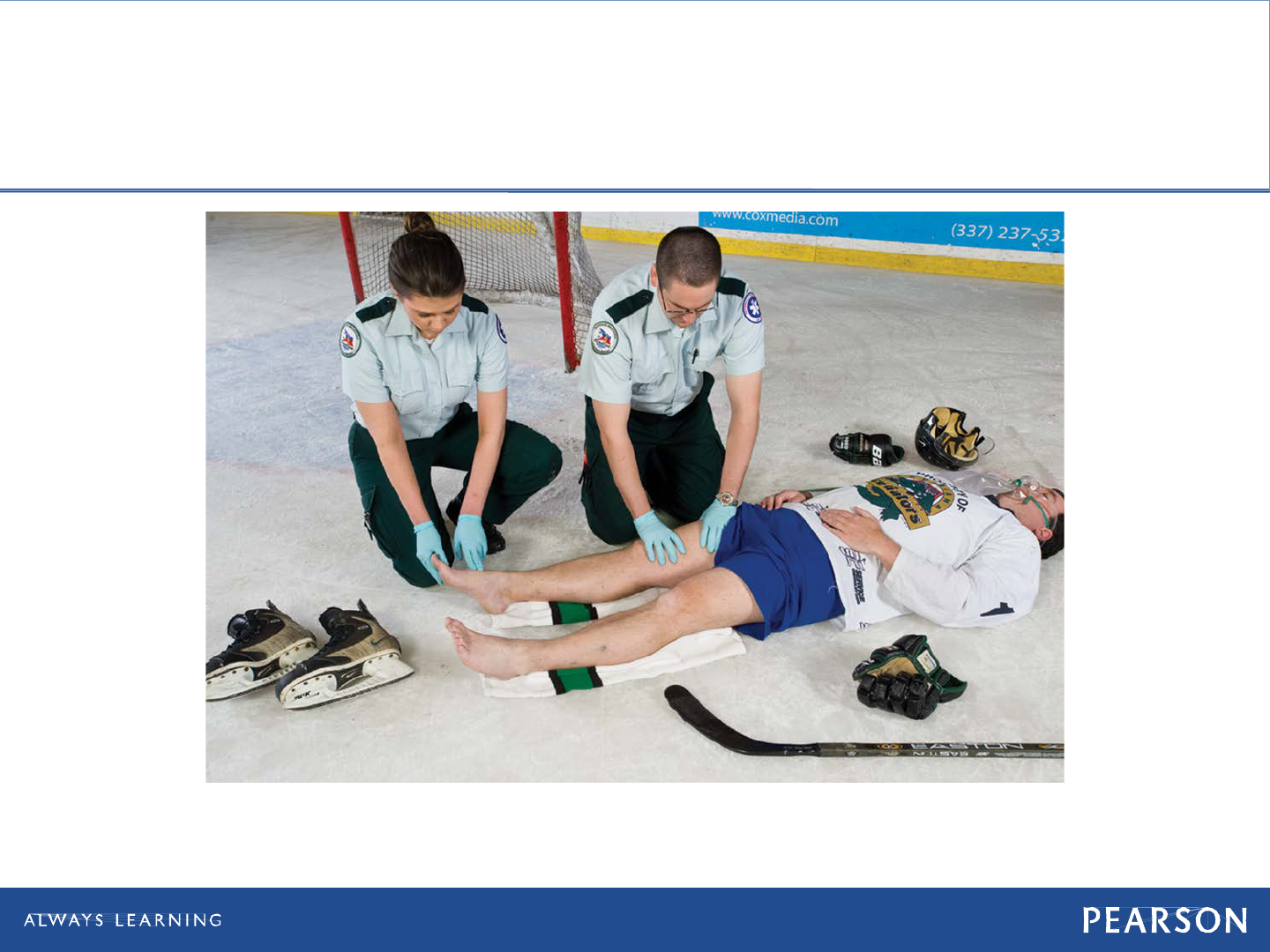
Traction Splint
• Take Standard Precautions and, if
possible, expose the area to be
splinted.
• Manually stabilize the leg and apply
manual traction.
• Assess CSM distal to the injury.
• Adjust the splint to the proper length,
and position it at or under the injured
leg.
continued on next slide

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Traction Splint
• Apply the proximal securing device
(ischial strap).
• Apply the distal securing device (ankle
hitch).
• Apply mechanical traction.
• Position and secure support straps.
continued on next slide

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Traction Splint
• Reevaluate the proximal and distal
securing devices, and reassess CSM
distal to the injury.
• Secure the patient's torso and the
traction splint to a long spine board to
immobilize the hip and to prevent
movement of the splint.
Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Treatment: Traction Splint
1. Take Standard Precautions. NOTE: Assess the distal circulation, sensation, and
motor function both before and after immobilizing or splinting an extremity.

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Treatment: Traction Splint
2. Manually stabilize the injured leg.

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Treatment: Traction Splint
4. Adjust the splint to the proper length, and position it next to the injured leg.

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Treatment: Traction Splint
8. Secure support straps, as appropriate.

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Emergency Care of Specific
Injuries

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Shoulder Girdle Injuries
• Patient assessment
Pain in shoulder
Dropped shoulder
Severe blow to back over scapula
continued on next slide

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Shoulder Girdle Injuries
• Patient care
Assess distal CSM.
Use sling and swathe.
If evidence of anterior dislocation of
head of humerus, place pillow between
patient's arm and chest.
Do not attempt to straighten or reduce.
Reassess distal CSM.

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Pelvic Injuries
• Patient assessment
Pain in pelvis, hips, groin, or back
Pain when pressure applied to iliac
crests
Cannot lift legs when lying on back
Lateral rotation of foot
Unexplained pressure in bladder
Bleeding from urethra, rectum, or
vaginal opening
continued on next slide

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Pelvic Injuries
• Patient care
Move patient as little as possible.
Determine CSM distal to injury site.
Straighten lower limbs to anatomical
position.
Stabilize lower limbs.
Assume spinal injuries.
continued on next slide

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Pelvic Injuries
• Patient care
Reassess distal CSM.
Care for shock, provide high-
concentration oxygen.
Transport patient as soon as possible.
Monitor vital signs.

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Pelvic Wrap
• Commercially available devices
Can also use a sheet
• Applied to patients who have pelvic
deformity or instability whether or not
signs of shock are present

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Pelvic Wrap
A commercial pelvic splint.
Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Pelvic Wrap
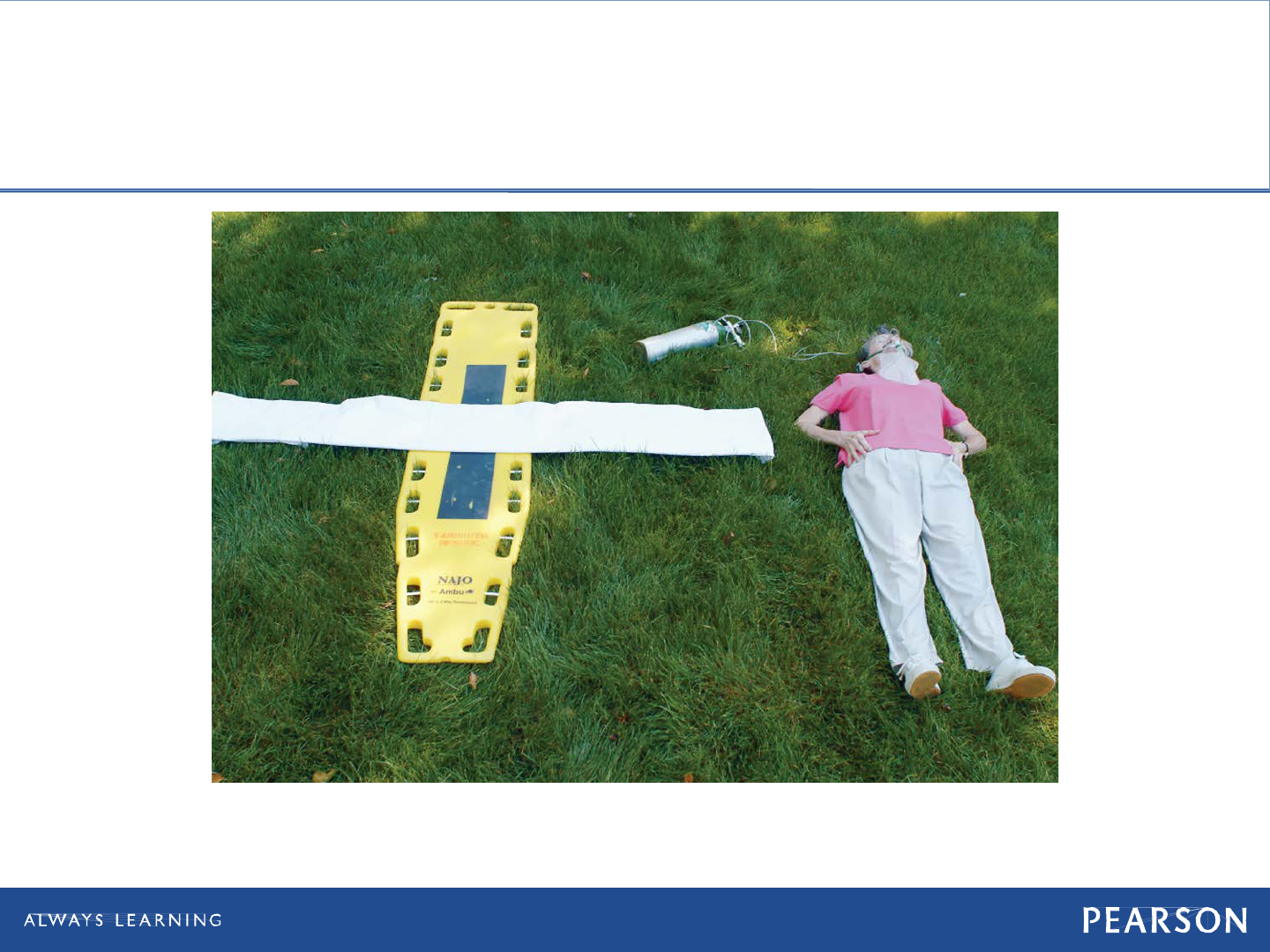
To devise a pelvic wrap, lay a sheet, folded flat, approximately 10 inches wide onto
the backboard.
Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Pelvic Wrap
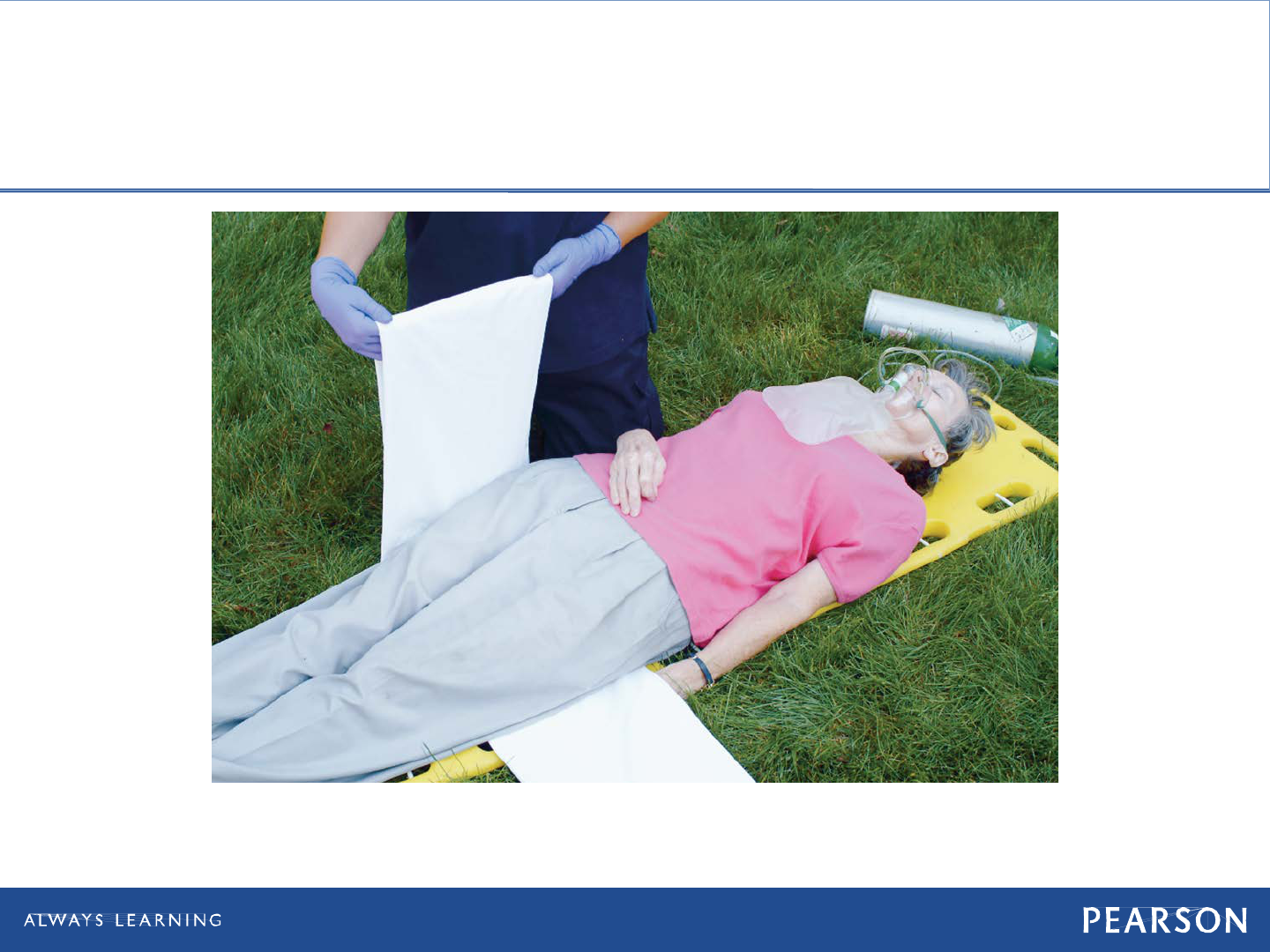
Bring the sides of the sheet together.
Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Pelvic Wrap
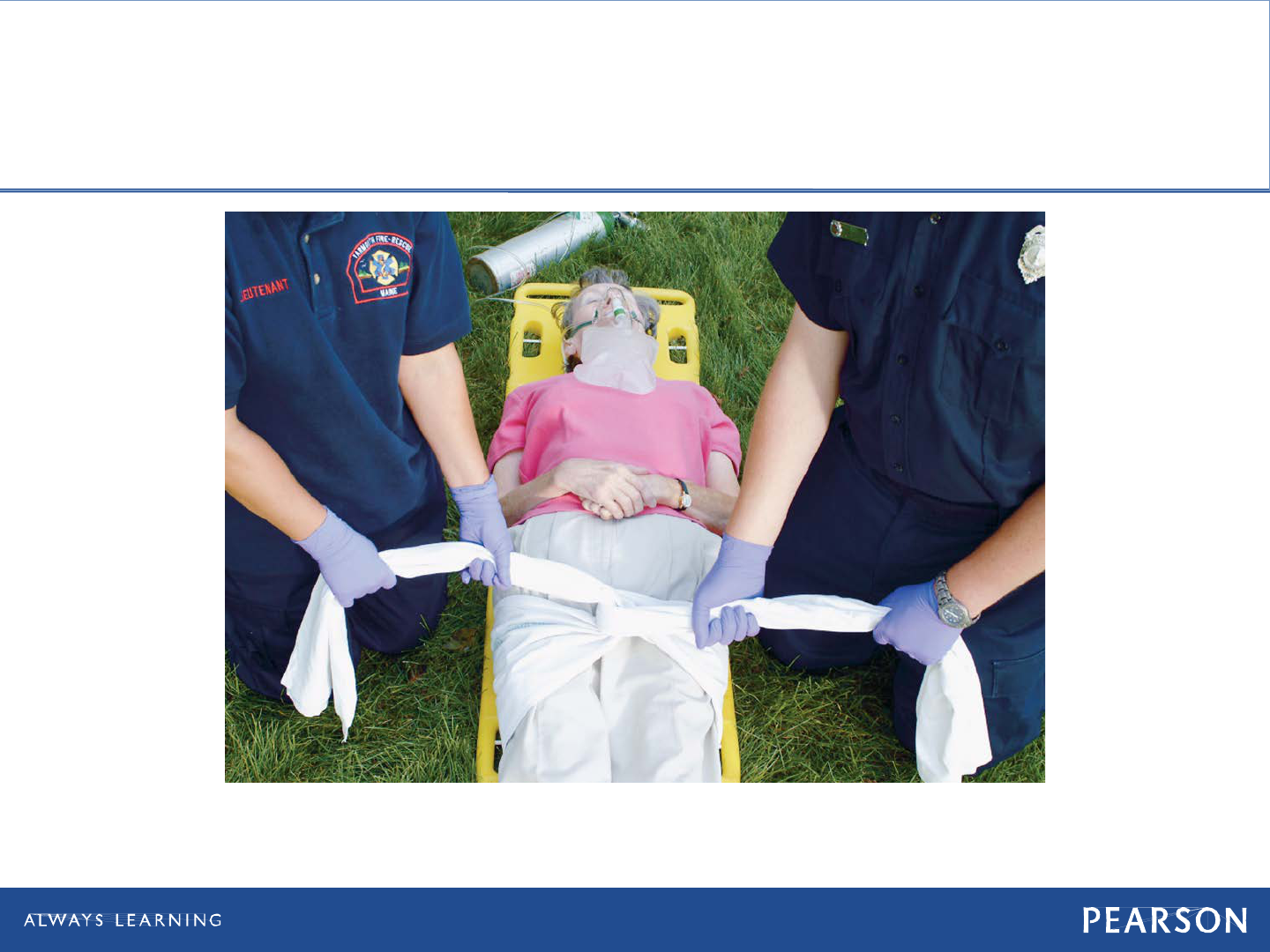
Tie the sheet firmly without overcompression to complete the pelvic wrap.

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
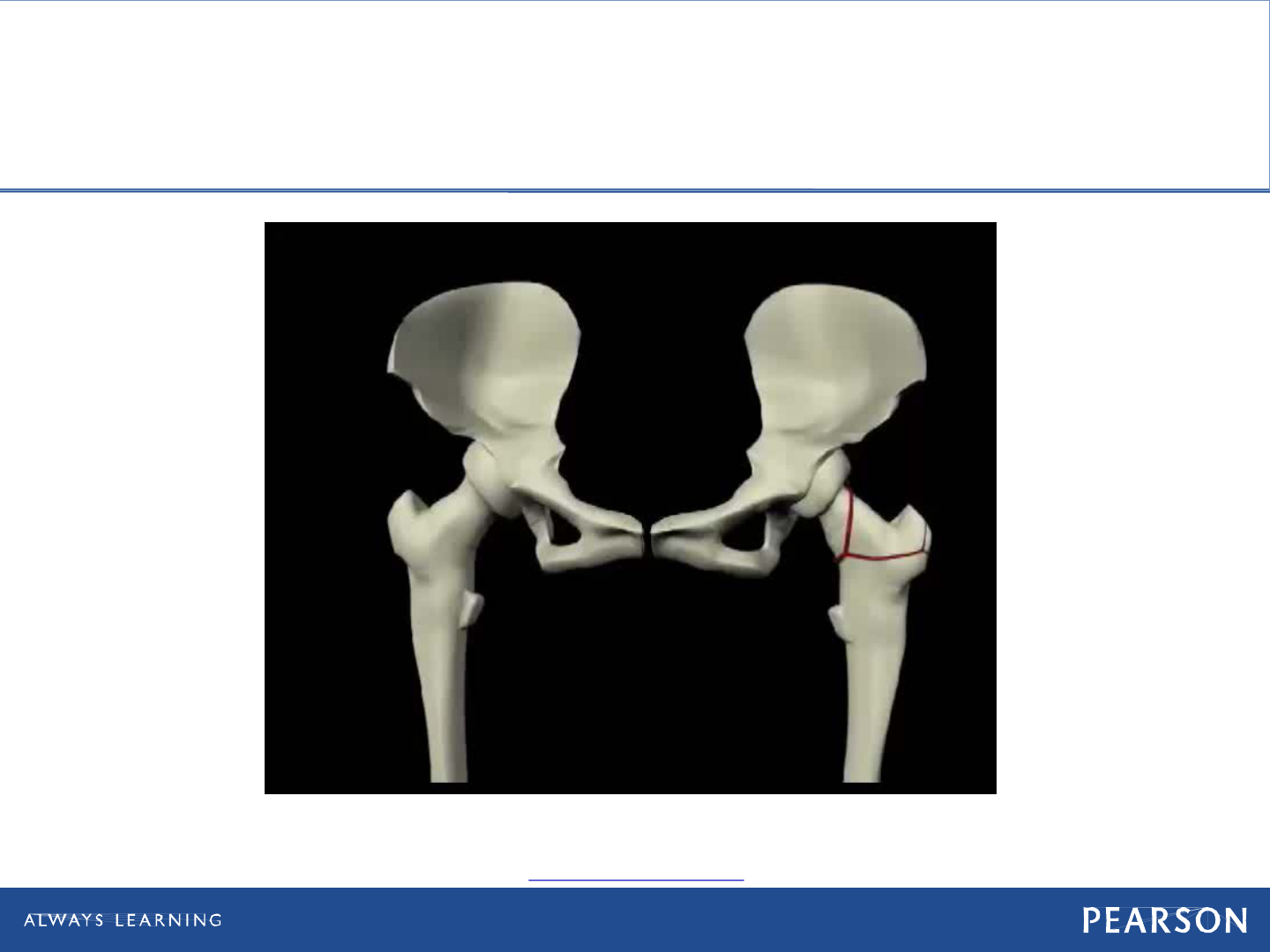
Hip Dislocation
• Patient assessment
Anterior hip dislocation
Posterior hip dislocation
• Rotation of leg inward and knee is bent.
• Foot may hang loose and unable to flex
the foot or lift toes.
• Lack of sensation in limb
continued on next slide

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Hip Dislocation
• Patient care
Assess distal CSM.
Move patient onto long spine board.
Immobilize limb with pillows and
blankets.
Secure patient to spine board.
continued on next slide

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Hip Dislocation
• Patient care
Reassess distal CSM.
Care for shock.
Transport, monitor vital signs, check for
nerve and circulation impairment.

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Geriatric Note
• Direct force and twisting forces can
cause a hip fracture.
MVC or falls
• Older adults are more susceptible to
this type of injury because of their
brittle bones or weakness from various
diseases.

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Hip Fracture
• Patient assessment
Pain is localized.
Surround tissues are discolored.
Swelling may be evident.
Unable to move limb while on back
Unable to stand
Foot on injured side turns outward.
Injured limb appears shorter.
continued on next slide

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Hip Fracture
• Patient care
Place folded blanket between patient's
legs, and bind legs together with wide
straps, or wide cravats.
Use thin splints to push cravats or
straps under patient at natural voids
and readjust so they will pass across
the chest, the abdomen just below the
belt, below the crotch, above and below
the knee, and at the ankle.
Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Hip Injuries
For a patient with a hip injury, bind the legs together.

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Femoral Shaft Fracture
• Patient assessment
Intense pain
Possibly open fracture
Injured limb may be shortened
continued on next slide

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Femoral Shaft Fracture
• Patient care
Control bleeding.
Manage for shock.
Provide oxygen.
Assess distal CSM.
Apply traction splint.
Reassess distal CSM.

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Pediatric Note
• When traction-splinting thigh injuries in
children, be sure to use appropriately-
sized splints.
• Infants and children with fractured
femurs often have injuries to internal
organs.

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Knee Injury
• Patient assessment
Pain and tenderness
Swelling
Deformity with swelling
• Patient care
Assess distal CSM.
Immobilize in current position.
Reassess distal CSM.

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Tibia or Fibula Injury
• Patient assessment
Pain and tenderness
Swelling
Possible deformity
• Patient care
Apply air-inflated splint.
Immobilize fracture using two rigid
board splits.
Apply single splint with ankle hitch.

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Ankle or Foot Injury
• Patient assessment
Pain
Swelling
Possible deformity
continued on next slide

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Ankle or Foot Injury
• Patient care
Assess distal CSM.
Stabilize limb.
Lift limb.
Place cravats under ankle.
Lower limb into pillow.
Tie pillow around ankle.

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Ankle/Foot Injury
A pillow splint may be used for an injured ankle.

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Ankle or Foot Injury
• Patient care
Tie fourth cravat at arch of foot.
Elevate with second pillow or blanket.
Reassess distal CSM.
Care for shock if needed.
Apply ice pack as needed.

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Forearm, Wrist, and Hand Injuries
• Signs
Forearm
• Deformity and tenderness
Wrist
• Deformity and tenderness
Hand
• Deformity and pain
• Dislocated fingers

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Splinting Forearm, Wrist,
and Hand Injuries
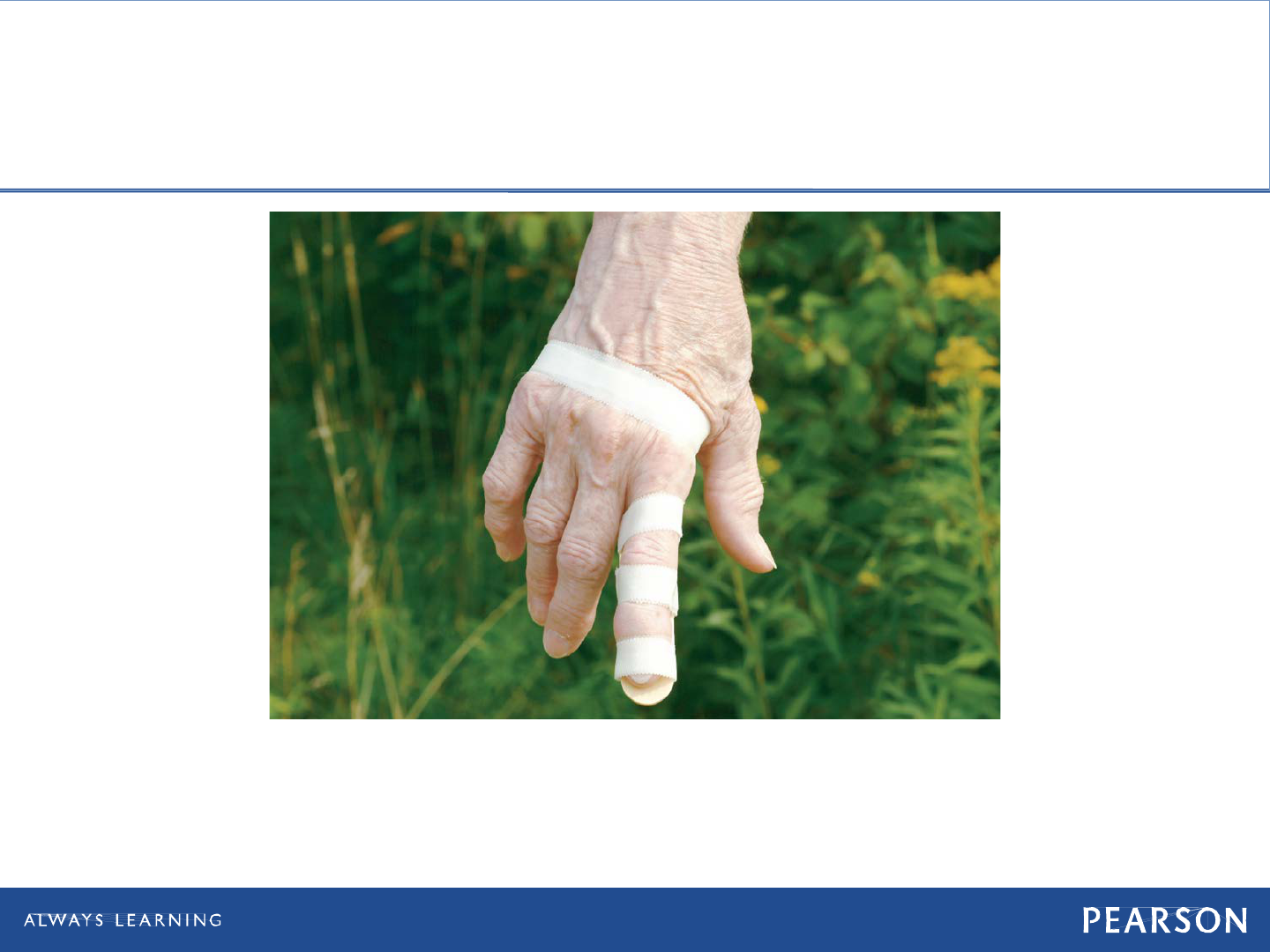
SPLINTING A FINGER: An injured finger can be taped to an adjacent uninjured finger,
which acts as a splint to the injured finger. Or an injured finger can be splinted with a
tongue depressor. Some emergency department physicians prefer that care to an
injured finger be limited to a wrap of soft bandages. Do not try to "pop" dislocated
fingers back into place.
Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Splinting Forearm, Wrist,
and Hand Injuries
SPLINTING A FINGER: An injured finger can be taped to an adjacent uninjured finger,
which acts as a splint to the injured finger. Or an injured finger can be splinted with a
tongue depressor. Some emergency department physicians prefer that care to an
injured finger be limited to a wrap of soft bandages. Do not try to "pop" dislocated
fingers back into place.

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Chapter Review

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Chapter Review
• Bones bleed. Fractures cause blood loss
within the bone as well as from tissue
damage around the bone ends. Serious
or multiple fractures can cause shock.
• Splinting of long-bone fractures
involves immobilizing the bone ends as
well as the adjacent joints.
continued on next slide

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Chapter Review
• Splinting protects the patient from
further injury, reduces pain, and helps
control bleeding.
• You may need to be creative while
splinting. There are many correct ways
to splint the same extremity.
• Injuries to bones and joints should be
splinted prior to moving the patient.
continued on next slide

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Chapter Review
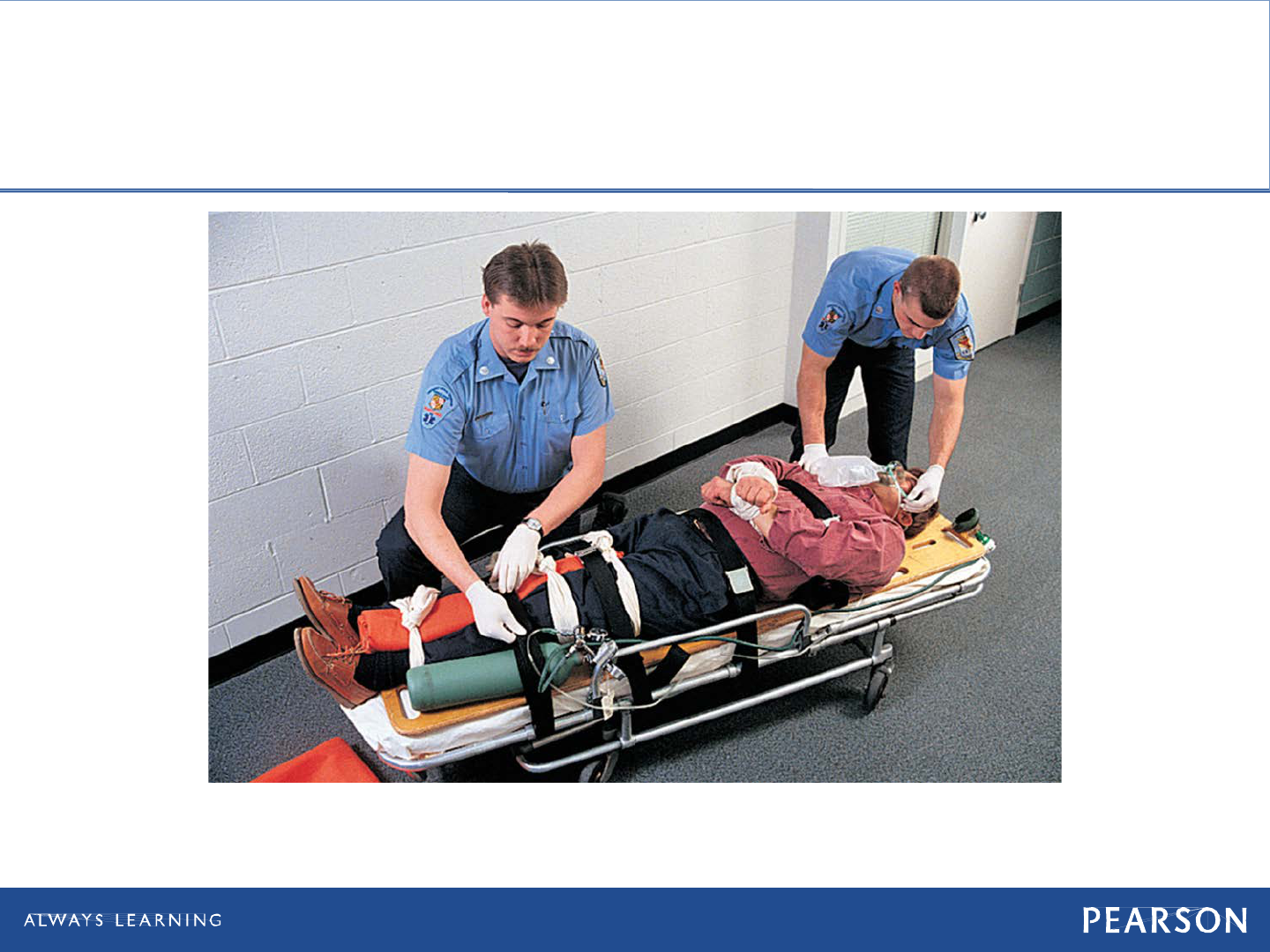
• If patient has multiple trauma or
appears to have shock (or a significant
potential for shock), do not waste time
splinting individual fractures. Place
patient on long spine board and secure
limbs to board. Splint individual
fractures en route if time and priorities
allow.

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Remember
• Bones, joints, muscles, cartilage,
tendons, and ligaments make up the
musculoskeletal system.
• Bones provide the body with structure,
store metabolic materials, and produce
red blood. Joints are the places where
bones articulate to create movement.
continued on next slide

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Remember
• Fractures, dislocations, sprains, and
strains are musculoskeletal injuries that
are caused by direct force, indirect
force, and twisting force. Injuries
should be splinted prior to moving the
patient.
continued on next slide

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Remember
• A closed extremity injury is one in
which the skin has not been broken. An
open extremity injury is one in which
the skin has been broken.
• Pelvic fractures and femoral shaft
fractures often indicate more severe
internal injuries.
continued on next slide

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Remember
• EMTs must learn specific techniques for
immobilizing particular injuries but at
the same time must foster creativity
while applying the general rules of
splinting.

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Questions to Consider
• Have I fully addressed life threats and
maintained my priorities even in the
presence of a grossly deformed
extremity?
• Does the patient have an injury that
requires splinting?
continued on next slide

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Questions to Consider
• Does the patient have multiple
fractures, multiple trauma, or shock?
• Does the patient have adequate CSM
distal to the musculoskeletal injury?
• Should I align the angulated extremity
fracture?

Copyright © 2016, 2012, 2009 by Pearson Education, Inc.
All Rights Reserved
Emergency Care, 13e
Daniel Limmer | Michael F. O'Keefe
Critical Thinking
• Patients who suffer fractures can be in
extreme pain. Pain can cause anxiety
and elevated pulse rates. How could
you differentiate between a patient with
a rapid pulse and anxiety from pain
versus a patient with rapid pulse and
anxiety from shock?